Released February 12, 2026
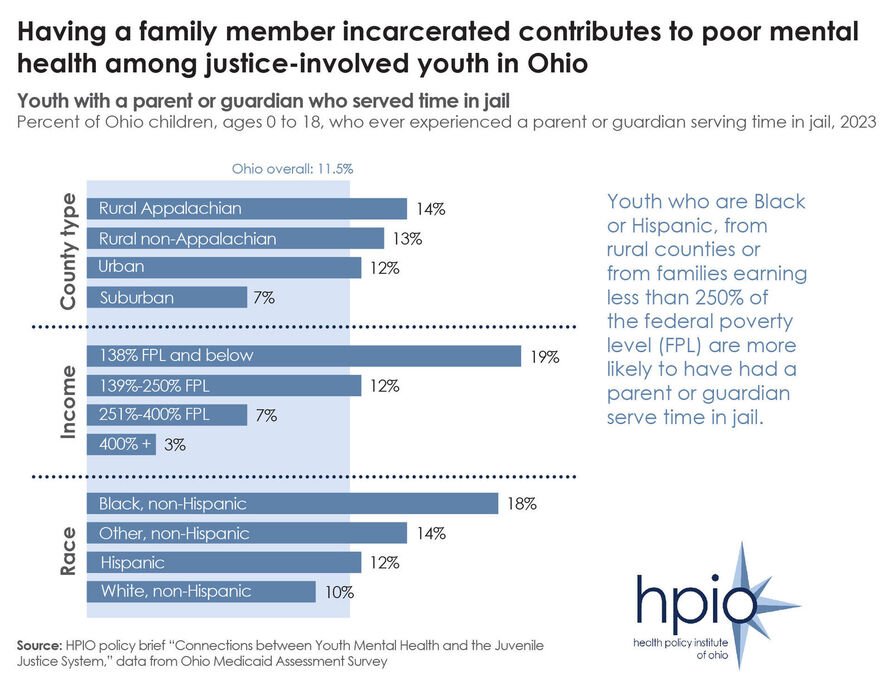
Data included in HPIO’s recently released policy brief on the Connections between Youth Mental Health and the Juvenile Justice System shows that Ohio youth who are Black or Hispanic, from rural counties and from families earning less than 250% of the federal poverty level (FPL) are more likely to have had a parent or guardian serve time in jail.
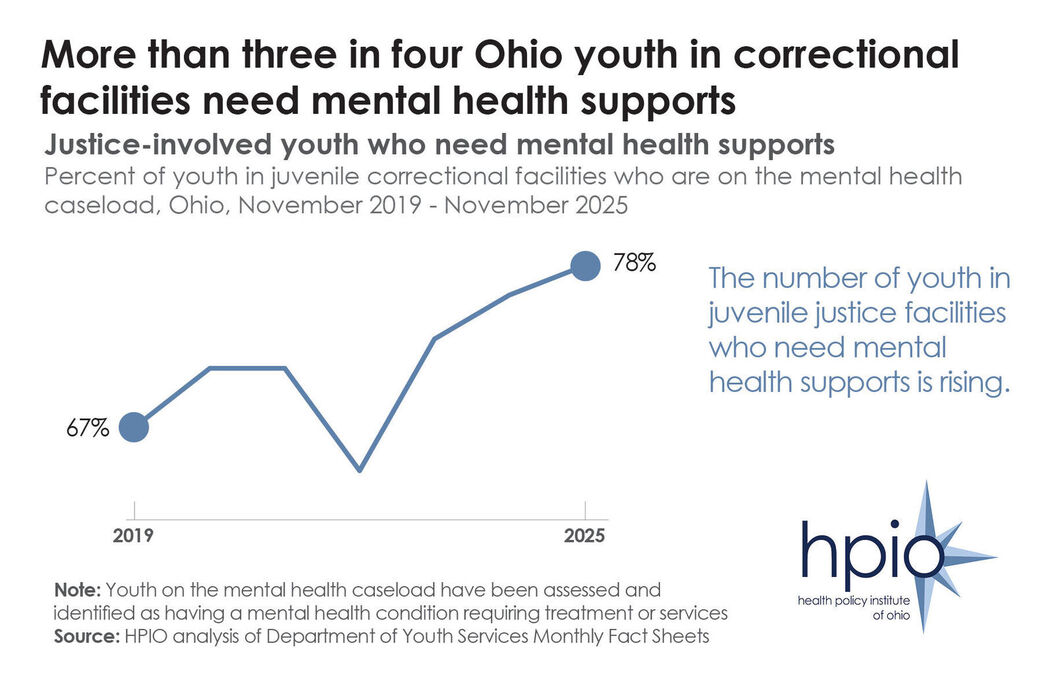
The brief found that there are several factors that contribute to poor mental health among children and teens, but some are more common among youth who become involved in the juvenile justice system, including adverse childhood experiences (ACEs).
Certain ACEs are more common among youth who become justice-involved, specifically sexual abuse, neglect and living in a household with someone who was incarcerated. According to HPIO’s Health Impacts of ACEs in Ohio brief, sexual abuse and incarceration of a household member are also two of the ACEs that have the most significant impact on the health of Ohioans.
The brief includes nine policy options that state policymakers can implement, and for which juvenile justice and child mental health partners can advocate, to improve mental health outcomes for at-risk youth and prevent justice involvement. The policy options, which were identified through a review of the U.S. Department of Justice Crime Solutions inventory, and through the expertise of the HPIO Child Mental Health advisory group, aim to prevent delinquent behavior, promote accountability, cultivate community safety and support the mental health of youth in detention or commitment.