Released June 06, 2025
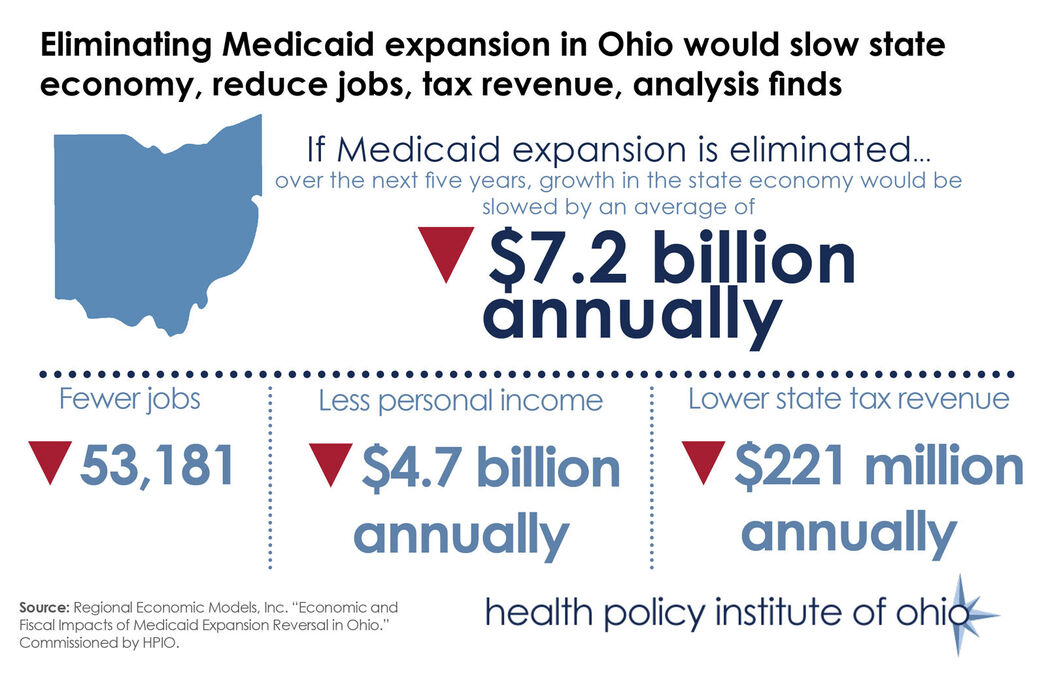
New analysis commissioned by the Health Policy Institute of Ohio projects that if Medicaid expansion is eliminated, growth in Ohio’s economy (i.e., the state’s gross domestic product) would decrease by an average of $7.2 billion annually, as illustrated above.
The analysis, conducted by Regional Economic Models, Inc., is the fifth and final in a series of briefs that are part of HPIO’s 2025 Ohio Medicaid Expansion Study.
According to the analysis, eliminating expansion would also slow job growth by more than 50,000 in Ohio, compared to if Medicaid expansion remained intact over the next five years. About 45% (more than 28,000) of the potential job losses would be in the healthcare sector and 55% would be spread widely across the state economy, including more than 6,400 construction jobs, more than 2,500 jobs in administrative and support positions and more than 2,000 restaurant jobs.
The study also found that “Ohioans would see an aggregate decline in personal income growth of $4.7 billion in an average year, representing more than $900 per household.”
Eliminating Medicaid expansion would also slow state tax revenue. “The growth in state general fund tax revenue would fall by an annual average of $220.6 million, with more than a quarter coming from the personal income tax and the remainder coming from a combination of sales taxes and the Commercial Activity Tax,” according to the study.
As this brief was developed, policymaking discussions at the federal level shifted. For example, reductions in the federal match for the Medicaid expansion population were not included in the bill passed by the U.S. House of Representatives on May 22, 2025. Still, other proposed changes could impact the availability of health coverage options for Ohio, such as proposed changes to the Federal Marketplace that would limit the timeframe in which Ohioans with lower incomes could enroll in insurance through the Marketplace. KFF has more information on proposed federal changes to health insurance policy.
At the same time, there are proposals from the Ohio General Assembly to incentivize Ohioans enrolled in Medicaid expansion into Marketplace coverage and a provision remains in the Ohio Senate-passed budget plan that would require Ohio to automatically discontinue Medicaid expansion if the federal match rate drops below the current 90% amount. Ohio policymakers need time and flexibility to make informed decisions that support every Ohioan reaching their full potential and make Ohio a model of health, well-being and economic vitality.