Released April 26, 2024
The Health Policy Institute of Ohio has released a new toolkit designed to provide partners with information about how to use evaluation to move towards equity.
Each section of “Moving Toward Equity: An Evaluation Toolkit,” covers a different element of evaluation, including information on how to tie evaluation into every step of assessment, planning, implementation and continuous quality improvement processes.
“There is much still to be done to ensure Ohioans of color, LGBTQ+ Ohioans, Ohioans with disabilities, Ohioans with low incomes, Ohioans living in urban, rural and Appalachian areas, and others can thrive in our state,” the toolkit states.
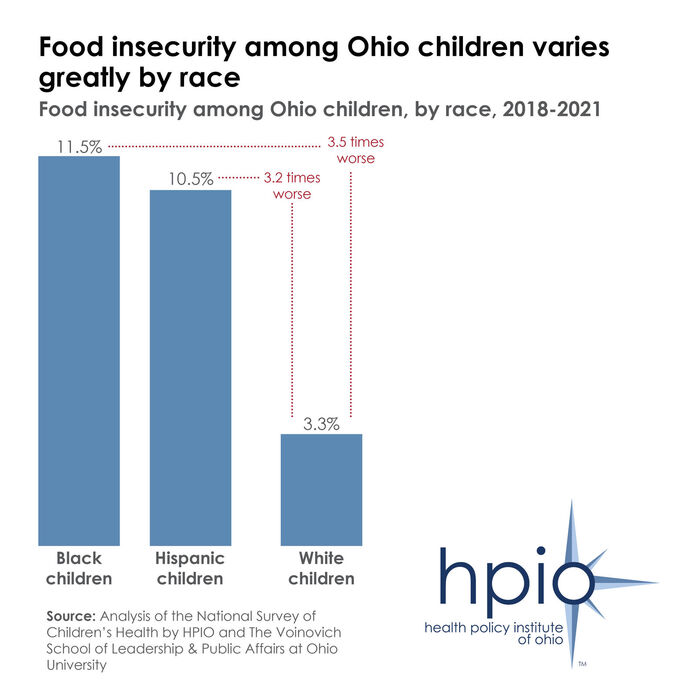
For example, HPIO’s 2024 Health Value Dashboard shows that Black and Hispanic Ohio children are much more likely to experience food insecurity than their white peers (as displayed above).
“An important part of this work is to evaluate and measure if our efforts to achieve equity are successful,” the toolkit states. “Evaluation tells us if what we’re doing is making a difference. It gives us the information needed to understand where we need to change, refocus or intensify our approaches. Perhaps more importantly, evaluation is also a process that can build trust, collaboration and accountability.”
The toolkit includes guidance, tools and resources on:
- Setting the stage for evaluation through assessment and planning
- Equitable approaches to evaluation
- Developing an equitable evaluation plan
- Using evaluation results for continuous quality improvement
- Collecting data for evaluation
The Toolkit is for anyone who is dedicated to advancing equity, passionate about achieving results and committed to stewarding resources. Tools are located in a separate workbook that is meant to be interactive and fillable, and can be accessed on the publication page.