Ohio addiction policy scorecard:
Overdose reversal and other forms of harm reduction
November 15, 2018
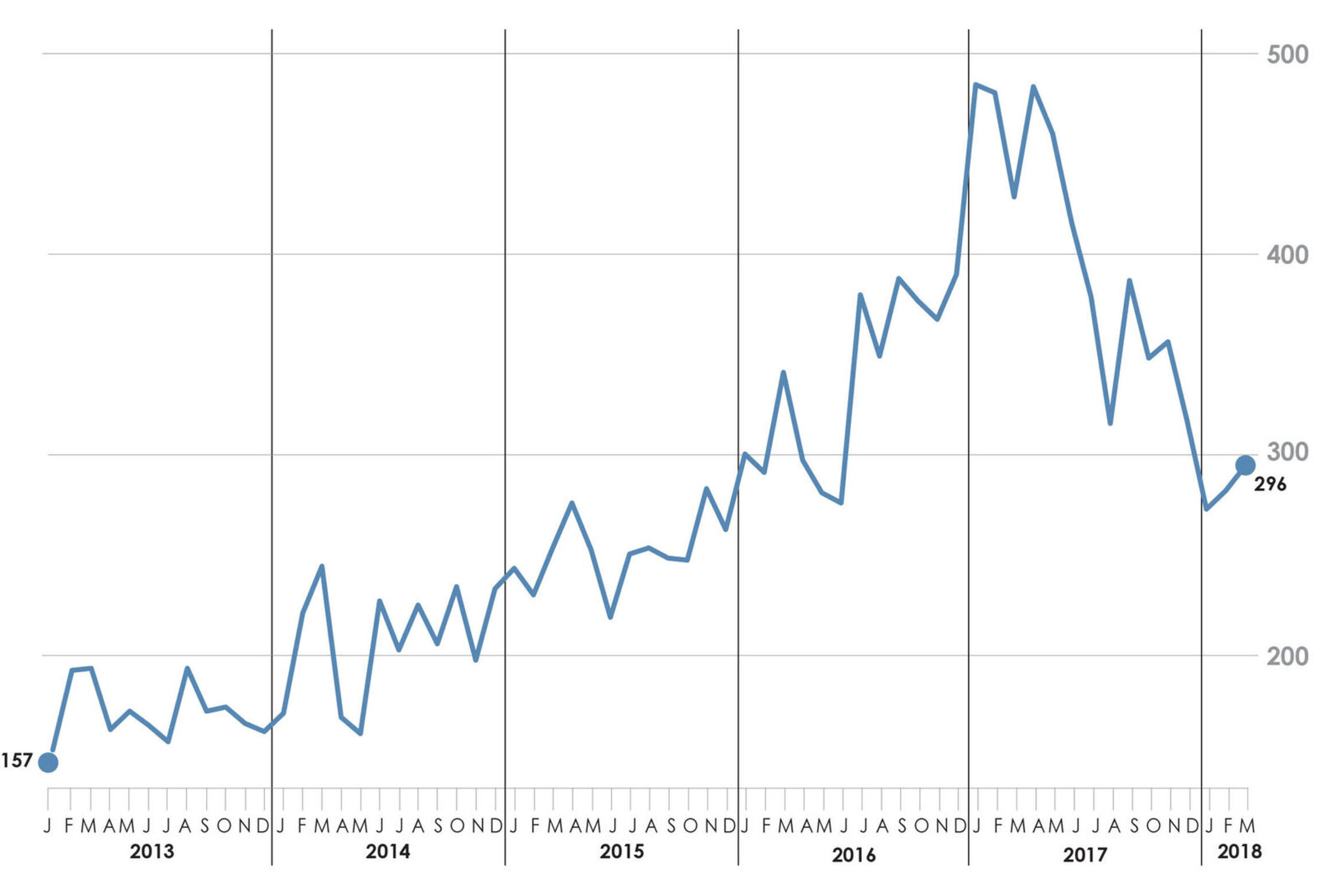
Drug overdose deaths are among the most visible and troubling signs of Ohio’s addiction crisis. Ohio has consistently had one of the highest drug overdose death rates in the country, with a total of 4,854 Ohioans dying in 2017. Newly-released data shows that deaths peaked in early 2017 and then declined (see figure ES 1 on page 2).
In addition to overdoses, many other addiction-related harms have increased dramatically in Ohio in recent years, such as the following downstream consequences of injection drug use:
- Hepatitis C is a liver disease caused by a virus that can be spread through needles and syringes used to inject heroin and other drugs. In 2016, 23,577 Ohioans were newly diagnosed with hepatitis C, up 49 percent from 2014.
- HIV, the virus that causes AIDS, can also be spread through shared needles. The number of new HIV diagnoses among people who inject drugs increased by 108 percent from 2013 to 2017 in Ohio
- Endocarditis is a bacterial heart infection associated with injection drug use. From 2008 to 2017, there was a 41-percent increase in endocarditis hospital encounters in Ohio.
Methamphetamine, cocaine, alcohol and tobacco use also have downstream harms, such as violence, property crime, homelessness, drunk driving crash deaths, child maltreatment and cancer.
Click to enlarge
Addiction-related harms are costly to state and local governments. For example, the state Medicaid program is paying to treat rising numbers of hepatitis C and endocarditis cases, and local governments are shouldering the costs of rising child welfare caseloads.
Harm reduction strategies can mitigate these consequences and related costs. The purpose of harm reduction is to save lives, improve the quality of life of people who use drugs and improve the overall health and safety of communities. While Ohio has embraced overdose reversal—one form of harm reduction—the state has been reluctant to act on other forms of harm reduction.
In order to provide policymakers and other stakeholders with the information needed to take stock of the policy response to addiction, this report reviews state-level policy changes related to overdose reversal and other forms of harm reduction enacted in Ohio from January 2013 to May 2018. It includes:
- An inventory of policy changes (legislation, rules and state agency initiatives, programs and systems changes)
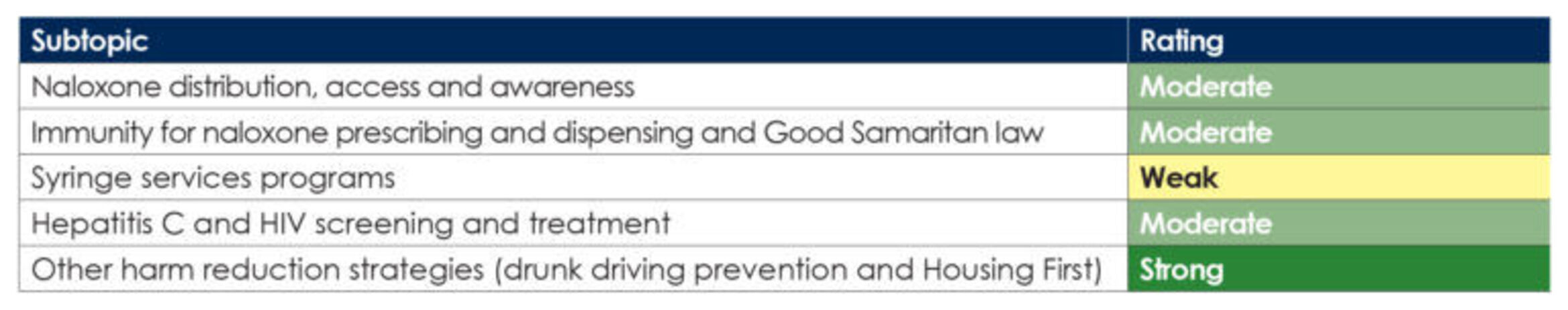
- A scorecard that indicates the extent to which Ohio is implementing strategies that are proven effective by research evidence (see figure ES 2 on page 3)
- Opportunities for improvement in both the public and private sectors
What is harm reduction?
Harm reduction is both a framework for understanding substance misuse and a set of policies and programs that aim to reduce the adverse health, social and economic consequences of drug use. Harm reduction addresses the conditions and consequences of drug use and incorporates a range of strategies, including safer drug use and abstinence, in order to meet the needs of all people with substance use disorder.
Figure ES1. Number of unintentional drug overdose deaths, Ohio, Jan. 2013 – March. 2018
What are the strengths of Ohio’s policy response?
State policymakers have focused on reversing the upward trend in overdose deaths in Ohio and have taken initial steps to reduce infectious disease rates and other harms associated with addiction. The following strengths stand out:
- Strong focus on overdose reversal. State policymakers have implemented several policy changes designed to increase the use of naloxone, the overdose reversal medication, including Project DAWN (Deaths Avoided with Naloxone) expansions and legal protections for professionals who dispense or administer naloxone.
- Initial steps to curb infectious disease associated with injection drug use. Ohio permits local health departments to establish syringe services programs (SSPs), and 18 counties now have SSPs.
- Efforts to reduce drunk driving. Ohio’s blood alcohol concentration laws are consistent with research-based recommendations, and Ohio law requires ignition interlocks for repeat offenders convicted of alcohol-impaired driving.
- Strong investment in Housing First. Ohio policymakers have emphasized a Housing First approach to rapid rehousing, including the Permanent Supportive Housing model, which has been expanded in Ohio over the past 10 years.
Figure ES 2. Summary scorecard rating: Extent to which Ohio policies and programs align with research evidence and reach Ohioans in need
What are the gaps in Ohio’s policy response?
Despite these strengths, Ohio continues to struggle with high drug overdose death rates and increasing rates of addiction-related harms, such as hepatitis C and HIV. In Ohio’s policy response to curb these trends, the following gaps remain:
- Barriers to naloxone. Some Ohioans still lack adequate access to naloxone. For example, there are at least 28 counties without a Project DAWN site, and some sites have limited programming. Community organizations and lay people face barriers to distributing or obtaining naloxone, largely due to the complexity of Ohio’s policies and lack of organizational capacity.
- Minimal prevention response to surge in hepatitis C cases. Despite sharp increases in the number of Ohioans with hepatitis C and the high cost of hepatitis C treatment, there are no significant statewide efforts to increase awareness, prevention, screening or treatment of hepatitis C. Eighty percent of Ohio counties do not have a syringe services program, including eight that are identified as high-risk for hepatitis C and HIV outbreaks.
- Life-saving hepatitis C treatment has been limited for Medicaid enrollees. Through 2018, Ohio Medicaid coverage for hepatitis C treatment has been inconsistent with clinical guidelines and more restrictive than Medicaid coverage in several other states. Starting in January 2019, an important restriction will be lifted, allowing patients to get treatment before experiencing serious health problems caused by liver disease.
- Harm reduction “deserts.” Seventeen rural Ohio counties have higher rates of addiction-related harms compared to other counties, but fewer harm reduction programs, such as Project DAWN sites and syringe services programs. Stigma and limited funding are likely keeping harm reduction strategies from being implemented in these communities.
Opportunities for improvement
Public and private partners in Ohio can work together to:
1. Continue to increase naloxone distribution across the state to ensure that all Ohioans have access to overdose reversal medication, including improved access for community organizations and lay people.
a. Increase the number of community sites that can distribute naloxone, including Project DAWN sites and other community-based organizations, so that there is better coverage across Ohio, particularly in counties with the highest overdose rates.
b. Expand the types of entities that are eligible to become Project DAWN sites, including non-profit organizations that serve people who inject drugs.
c. Allow community organizations to distribute naloxone without a Terminal Distributor of Dangerous Drugs (TDDD) license and/or provide assistance to entities so that they can obtain a TDDD license.
d. Increase naloxone distribution by continuing to integrate Project DAWN and other distribution models with addiction treatment settings, re-entry from prison and jail and SSPs.
e. Establish additional methods for distributing naloxone in the community, such as by storing and maintaining naloxone in automated external defibrillator (AED) cabinets.
f. Simplify Ohio’s Good Samaritan law and reduce the restrictions on Good Samaritan immunity so that bystanders are encouraged to call for help during an overdose.
g. Create civil liability protections for lay persons who administer naloxone to a person experiencing an overdose.
h. Expand the current media campaign to inform the public, including drug users, family members and friends of drug users and community groups, of the availability of naloxone, Ohio’s Good Samaritan law and other legal immunities related to naloxone distribution and administration.
i. Increase the sustainability of the Project DAWN program by establishing a pathway for Project DAWN sites to bill insurance providers for the naloxone they distribute.
2. Launch an intensive initiative to reduce the spread of infections associated with injection drug use, including increased awareness of the importance of prevention, treatment and harm reduction.
a. Create an integrated state plan to reduce hepatitis C transmission and reinfection, similar to the Ohio HIV Prevention and Care Integrated Plan.
b. Increase the number of syringe services programs in Ohio, particularly in counties with the highest rates of hepatitis C and HIV.
c. Identify sustained funding sources to support syringe services programs and explore ways to capture downstream savings to Medicaid and the Ohio Department of Rehabilitation and Correction (DRC) to reinvest in infection prevention.
d. Establish a statewide coordination hub for syringe services programs that can assist local programs with information sharing, technical assistance, evaluation and quality improvement.
e. Develop a campaign to reduce stigma for harm reduction approaches.
3. Continue to improve access to hepatitis C treatment for Medicaid enrollees, while exploring strategies to control treatment costs.
a. Remove or reduce restrictions related to sobriety timeframes and specialist providers.
b. Engage primary care providers, including Federally Qualified Health Centers (FQHCs), in providing direct-acting antiviral (DAA) treatment for patients with hepatitis C.
c. Increase screening efforts for hepatitis C and HIV across the state, particularly for priority populations, including people who inject drugs.
d. Implement strategies identified by the National Governor’s Association to ensure fiscal sustainability of hepatitis C treatment in the Medicaid program, such as by incorporating value assessments into policies and purchasing approaches.
In addition, state policymakers can do more to:
4. Reduce the number of alcohol/drug-impaired motor vehicle crashes.
5. Improve surveillance and evaluation to ensure that the state is investing in effective strategies.