- Posted
- October 17, 2025
Graphic of the week: Medicaid cost-sharing requirement
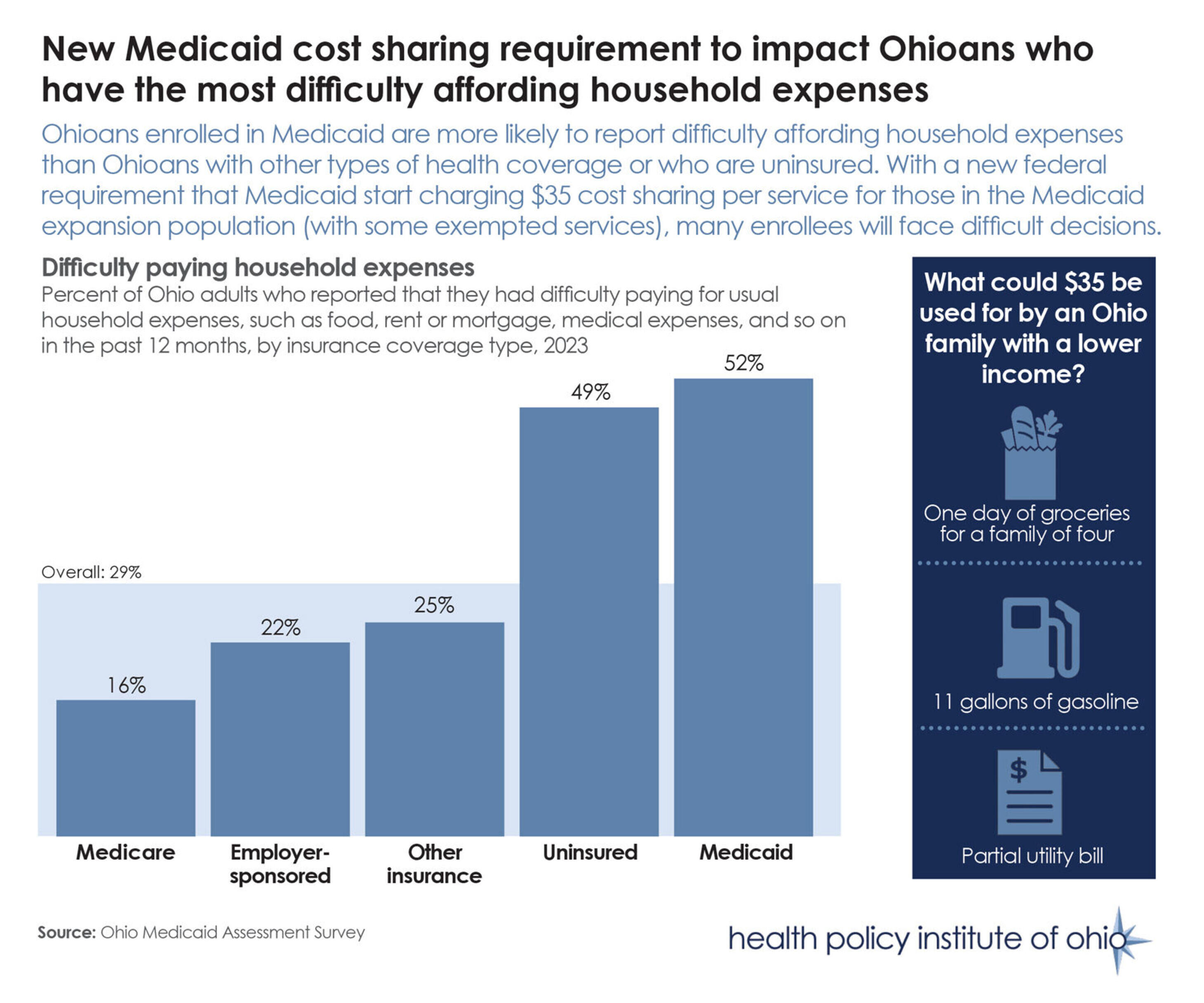
HR 1, the federal reconciliation bill (sometimes referred to as the “One Big Beautiful Bill Act”) that passed Congress over the summer, includes a requirement that states impose cost sharing of up to $35 per service for some Medicaid expansion enrollees.
As illustrated above, Ohioans who are enrolled in Medicaid are more likely to report difficulty paying household costs, such as food, housing and medical expenses, than those with other forms of insurance or those who are uninsured.
The new cost-sharing requirement is set to go in effect on Oct. 1, 2028, and includes co-pays, co-insurance and deductibles. The requirement will apply to all Medicaid enrollees earning between 100% and 138% of the federal poverty level ($32,150 to $42,759.50 for a family of four in 2025).
Primary care, mental health and substance use disorder services will be excluded from the cost-sharing requirement, as will services provided by federally qualified health centers, behavioral health clinics and rural health centers.
HPIO has developed a series of publications to explore the healthcare access and affordability impacts of recent policy changes, such as HR 1 and the state’s biennial budget bill.