Medical Marijuana in Ohio
updated 09.21.2017
Purpose: To inform policymakers and other stakeholders about the Medical Marijuana Control Program and medical marijuana legalization in Ohio, including descriptions of:
- House Bill 523
- State regulations of marijuana growth, distribution and use
- State vs. federal legal considerations
This resource page also includes resources on the health and policy implications of changes in marijuana use.
This resource page provides a summary of changes to Ohio law for informational purposes only and is not intended to be a comprehensive statement of law or policy.
Background: In November 2015, Ohio voters rejected a ballot initiative that would have amended the Ohio State Constitution to legalize medical and recreational marijuana use. Although the ballot issue did not pass, discussions of the ballot issue revealed strong public interest in changing marijuana policy in Ohio. In response, the Ohio General Assembly passed House Bill 523 (HB 523), which became effective on Sept. 8, 2016, legalizing medical marijuana in the state.
As Ohio’s new medical marijuana program is rolled out and fully implemented, there will likely be opportunities for policymakers to consider additional policy changes to revise or improve current marijuana policy. The following information and resources are intended to help interested policymakers and other stakeholders understand the current state of the law in Ohio and at the federal level, and the ongoing policy and health implications of the legalization of medical marijuana.
State law vs. federal law
Ohio is one of 20 states plus the District of Columbia that has decriminalized possession of small amounts of marijuana, making possession under a certain weight a misdemeanor crime. Twenty-nine states and the District of Columbia have state laws allowing the medical use of marijuana. With the passing of House Bill 523, Ohio is now one of these states. Additionally, eight states and the District of Columbia have legalized the recreational use of marijuana.
Despite decriminalization and legalization at the state level, marijuana remains illegal at the federal level and is classified as a Schedule I substance under the Controlled Substances Act (CSA) of 1970. Schedule I drugs are those considered by the federal government to have high potential for abuse, no accepted medical use in the U.S. and a lack of accepted safe use of the drug under medical supervision. 1 However, there are conflicts between state and federal scheduling. Although marijuana is a Schedule I substance federally and in other contexts in the state of Ohio2, it is considered a Schedule II substance for the purpose of Ohio’s Medical Marijuana Control Program.3 A Schedule II substance is defined by the CSA as a substance that has a high potential for abuse, but has some accepted medical use.
In October 2009, the U.S. Department of Justice announced formal guidelines for federal prosecutors in states with enacted laws authorizing the use of medical marijuana. The guidance stated the Department’s commitment to enforcement of the CSA, but noted that federal resources would not be directed at prosecuting individuals whose actions were clearly and unambiguously in compliance with state laws allowing medical marijuana use. An updated statement, commonly known as the “Cole memorandum,” was released in August 2013 in response to state ballot initiatives legalizing recreational use of marijuana. The guidance provided that the Department would not devote resources to prosecuting crimes involving possession of small amounts of marijuana for personal use on private property.
The U.S. Congress has previously taken action to protect state medical marijuana laws as well. The Rohrabacher-Farr amendment, which was passed as part of an omnibus spending bill in 2014, prohibited the use of federal funds to prevent states from “implementing their own state laws that authorize the use, distribution, possession or cultivation of medical marijuana.”4 The Ninth Circuit Court of Appeals ruled that this amendment barred the federal government from taking legal action against any individual involved in medical marijuana-related activity absent evidence that the defendant is in clear violation of state law. However, the Rohrabacher-Farr amendment does not amend the CSA and must be re-authorized annually to stay in effect. In an emergency aid package passed by Congress in Sept. 2017, the Rohrabacher-Farr amendment was extended until Dec. 8, 2017. It is unclear how Congress will proceed on this issue in the future.
In addition to the law enforcement complications of conflicting state and federal marijuana laws, businesses and policymakers in states legalizing marijuana for medical or recreational use have to navigate questions related to a diverse range of other issues, including packaging, labeling, banking regulations and advertising.
The Medical Marijuana Control Program and medical marijuana in Ohio
Medical marijuana law in Ohio
Ohio House Bill 523 (“HB 523”) legalized medical marijuana in the state of Ohio on September 8, 2016.5 HB 523 created the Medical Marijuana Control Program6, which allows patients who have been diagnosed with certain qualifying conditions, and who have the recommendation of a certified physician, to purchase and use medical marijuana. The Medical Marijuana Control Program will be fully functional as of Sept. 8, 2018.7 It is being developed by the Ohio Department of Commerce, Ohio Board of Pharmacy (“Pharmacy Board”) and State Medical Board of Ohio (“Medical Board”)8, who have written regulations with the input of the Medical Marijuana Advisory Committee and the general public. The Department of Commerce, Pharmacy Board and Medical Board work in collaboration to oversee marijuana growers, labs, processors, dispensaries, patient registration and physician certification.9
HB 523 also created the Medical Marijuana Advisory Committee, which is comprised of representatives from a variety of interested fields, including medicine, pharmacy, labor, law enforcement, patient advocacy and others. The committee advised and made recommendations to the Department of Commerce, Pharmacy Board and Medical Board on the development of the regulations for the Medical Marijuana Control Program.
For more information, see the Medical Marijuana Control Program website
Patients
Medical marijuana patients will be registered through the Ohio Board of Pharmacy (“Pharmacy Board”) no later than September 2018. Patients will be able to purchase and use medical marijuana if it is recommended by a certified physician and the patient has been diagnosed with at least one of the 21 qualifying conditions (see figure 1).10
Individuals also have the ability to petition the State Medical Board of Ohio (“Medical Board”) to add conditions to this list.11 A petition must specify the exact disease or condition that should be added as a qualifying condition, as well as scientific evidence and other information from experts supporting the addition of the condition. The applicant is asked to consider whether “conventional medical therapies” are insufficient to treat the condition, and must provide scientific evidence supporting the use of medical marijuana as treatment for the specific condition.12
Patients are not permitted to smoke medical marijuana, but may obtain marijuana in tincture, plant material, patch or edible form. Unlike some other states, patients in Ohio may not purchase full marijuana plants or seedlings. Edible forms of medical marijuana must be distinguishable so that they are not accidentally consumed by children.13 Minors are permitted to use medical marijuana if the recommending physician receives parental consent.14 Patients may only obtain a 90-day supply of medical marijuana at one time,15 and the amount of medical marijuana that constitutes a 90-day supply is defined in regulations by the Pharmacy Board (see figure 2).16
Patients and caregivers must register with the Pharmacy Board in order to purchase medical marijuana. The annual registration fee for patients is $50, and the annual fee for caregivers is $25.17 Caregivers must 21 years old or older, and cannot care for more than two patients who are treated with medical marijuana at a time. Patients are unable to have more than two caregivers, unless end of life care requires more than two caregivers or the caregivers and patients are members of the same household.18
Currently, patients registered in the state of Ohio to use medical marijuana are not permitted to purchase marijuana in other states. However, the Pharmacy Board may reach agreements with other states whose medical marijuana eligibility criteria are similar, allowing patients to buy marijuana in both states.
Although patients may legally purchase medical marijuana with the recommendation of a physician, they are not permitted to operate a vehicle, streetcar, trackless trolley, watercraft or aircraft while under the influence of medical marijuana.19
Final patient and caregiver rules
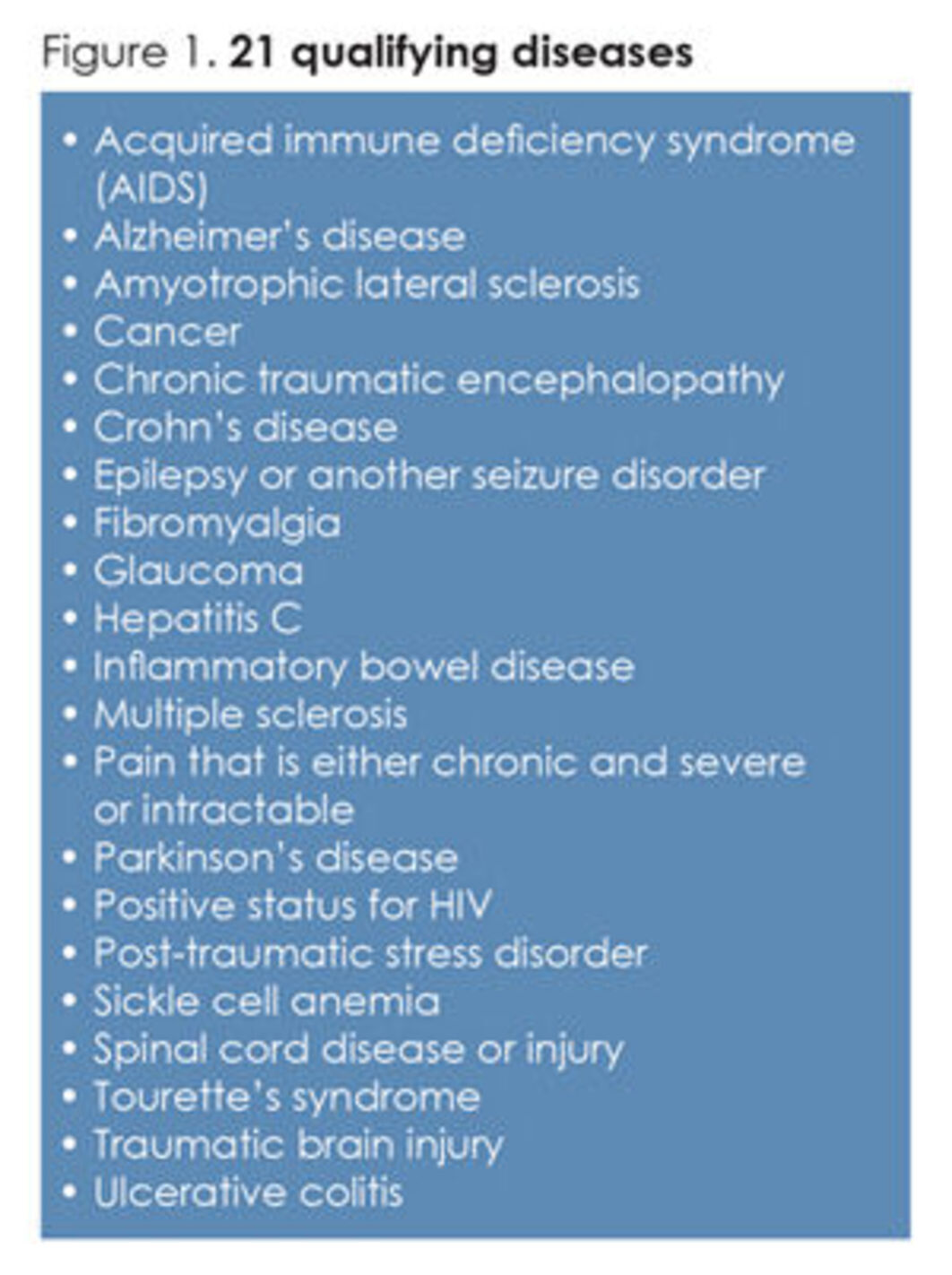
Fig 1. 21 qualifying diseases
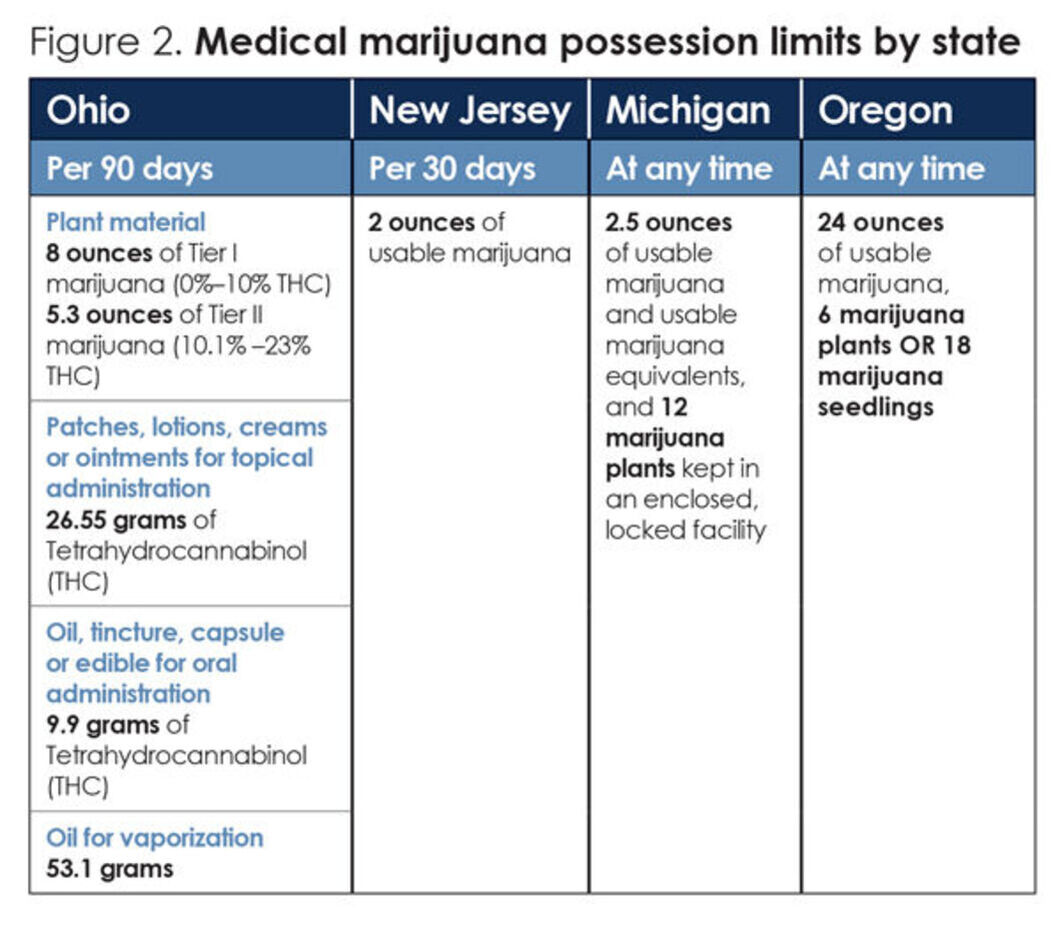
Fig. 2. Medical marijuana possession limits by state
Physicians
Physicians who choose to recommend medical marijuana must be certified by the State Medical Board of Ohio (“Medical Board”) to recommend medical marijuana to patients. Because marijuana is a Schedule I substance under federal law, physicians cannot prescribe medical marijuana to their patients. They may only “recommend” that their patients purchase and use marijuana legally under state law. Only physicians may recommend medical marijuana in Ohio. Once a physician is certified to recommend medical marijuana, that certification must be renewed on a biennial basis along with the physician’s medical license.20
Before recommending marijuana to a patient, Ohio law requires a “bona fide” physician-patient relationship be established. This means that the patient must be diagnosed with at least one of the conditions that legally qualify him or her to access medical marijuana, the patient must have a physical examination and medical history review performed by the recommending physician and an ongoing treatment regimen must be established.21
In order to maintain their certification to recommend medical marijuana, physicians must complete at least two hours of continuing education in diagnosing the qualifying medical conditions or treating those conditions with medical marijuana.22 This continuing education requirement is meant to ensure that physicians can diagnose the qualifying conditions, create and implement a medical marijuana regimen with the patient and understand potential drug interactions with medical marijuana. Continuing education courses for medical marijuana must be certified by the Ohio State Medical Association (OSMA) or the Ohio Osteopathic Association.
Click here for more information from OSMA about certification of medical marijuana courses.
Even though marijuana is prohibited federally, Ohio state law provides that physicians are not subject to criminal prosecution, are immune from civil liability and are not subject to professional disciplinary action for advising a patient about the benefits and risks of medical marijuana, recommending that a patient use medical marijuana to treat or alleviate a qualifying condition or monitoring a patient’s treatment with medical marijuana.23 However, recommending physicians may be subject to professional disciplinary action if they personally dispense medical marijuana or issue a recommendation to themselves or their family members.24
Dispensaries
Medical marijuana dispensaries are overseen by the Ohio Board of Pharmacy (“Pharmacy Board”). The Pharmacy Board will release 60 provisional licenses to dispensaries before September 8, 2018.26 When determining the distribution of these dispensaries throughout the state, the Pharmacy Board was required to consider the population distribution and the demand of medical marijuana throughout the state, with the purpose of making medical marijuana accessible to all potential patients.27 With these factors in mind, the Pharmacy Board will issue provisional licenses to 10 dispensaries in northwest Ohio, 18 in northeast Ohio, 17 in southeast Ohio and 15 in southwest Ohio (see figure 3). Most central Ohio counties are split between the southeast and southwest regions.
Medical marijuana dispensary districts
In order to be operational, a dispensary must employ a pharmacist, physician or other provider with prescribing powers to act as the clinical director. The clinical director will educate employees and be on-call during operating hours. When a sale of medical marijuana is made, dispensary employees are required to report the sale within five minutes to the Ohio Automated Rx Reporting System (OARRS). Medical marijuana must be purchased from a dispensary, and the home delivery of medical marijuana is prohibited.28
A dispensary cannot be built within 500 feet of a school, library, church, public playground or park, and if one of these structures is built within 500 feet of a preexisting dispensary, the Department of Commerce and Pharmacy Board will determine whether the dispensary can remain, must relocate or will have its license revoked.29
Dispensary fee structure:25
- Application for license: $5,000
- Certificate of operation: $70,000
- Dispensary associate key employee: $500
- Dispensary key employee: $250
- Dispensary support employee: $100
- Biennial renewal for dispensary license: $70,000
- Change of ownership: $5,000
- Relocation: $5,000
- Major modification or renovation: $5,000
- Advertising approval: $100 per ad
Fees paid to Ohio Board of Pharmacy
Cultivators and processors
Medical marijuana may only be grown within a government-sanctioned facility. The Department of Commerce will initially disperse 24 licenses for growing facilities. This will include 12 Level I licenses and 12 Level II licenses, with more distributed as the Department of Commerce sees fit. The license levels are differentiated by the size of the facility, application fee and liquid assets required of the applicant. In both level categories, the fees are substantial, which may limit the number of small businesses that apply. During the first application period in June 2017, 185 applicants applied for the 24 cultivator licenses that are available.30
List of organizations that applied for cultivator licenses in 2017
Application for a cultivator license is a competitive bidding process. Applicants are asked to include a business plan and operational policies and procedures as part of their application. Experience with the cultivation of medical marijuana is part of the application, which may favor out-of-state applicants.
Once marijuana is harvested by the cultivators, processors create the consumable products. The Department of Commerce may issue up to 40 processor provisional licenses prior to September 9, 2018. The cost of obtaining a processor license is substantial. The application fee is $10,000, certificate of operation fee is $90,000 and the annual license renewal fee is $100,000.
Medical marijuana in the workplace
HB 523 states that employers are not required to accommodate an employee’s medical marijuana usage and are permitted to establish a drug-free workplace policy or require routine drug testing. If a drug-free policy is not established in the workplace, no adverse employment action can be taken against an employee for their use of medical marijuana. If a drug-free workplace policy is established, an employer may take adverse employment action against an employee for their medical marijuana usage. If that employee is terminated, they are ineligible to take legal action against their employer.
If the injury or death of an employee under the influence of medical marijuana occurs in a workplace with a drug-free policy, neither the employee nor their dependents are eligible to receive workplace compensation.31
Monitoring and evaluation
The Medical Marijuana Control Program is monitored through the Ohio Automated Rx Reporting System (OARRS). Dispensaries are required to report each sale of medical marijuana to OARRS within five minutes of the sale. That report includes, among other information, the patient registry identification number, the name of the recommending physician and the quantity of marijuana purchased.32 The Ohio Board of Pharmacy (“Pharmacy Board”) is required to create a semi-annual report of the information collected from OARRS, which will be publicly available on the Pharmacy Board’s website.
Dispensary employees also have a duty to monitor suspicious recommendations and unusual usage of medical marijuana.33 Pursuant to this duty , dispensary employees must notify the Pharmacy Board in the case of unexplained product losses, security breaches and all other known violations of state drug laws. In the case of theft or fraudulent recommendation, the dispensary must notify the Pharmacy Board and law enforcement.
Additionally, physicians who recommend medical marijuana are required to submit an annual report to the State Medical Board of Ohio (“Medical Board”) that describes the physician’s observations regarding the effectiveness of medical marijuana in treating the physician’s patients over the previous year.
Health effects of marijuana use
While some research has been done on the medical use and effectiveness of marijuana and its derivatives, research is limited by the drug’s federal classification as a Schedule I substance. Because of this classification, researchers must be licensed by the Drug Enforcement Administration (DEA) and must obtain research-grade marijuana through the National Institute of Drug Abuse. Both federal agencies have lengthy processes for gaining needed approval and access that present a significant barrier to researchers looking to study the potential medical uses of marijuana.
- The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research
This 2017 report from the National Academies of Sciences, Engineering, and Medicine presents a review of the research published after 1999 about recreation and therapeutic marijuana use. The report provides evidence based recommendations and research conclusions about the health effects of marijuana use.
- Prevalence, reasons, perceived effects, and correlates of medical marijuana use: A review
This 2017 literature review analyzed 25 articles and described the marijuana use statistics in those articles. The review found that the main reason for medical marijuana use was pain management, typically being chronic pain and/or pain from multiple conditions. The comparison of marijuana use for pain versus opioid use is discussed briefly, although the authors call for more research to provide evidence to inform pain management techniques. The review indicated that many patients seeking a medical marijuana prescription were individuals who had previously used marijuana, so they may have a lower perceived risk. The literature review also showed that medical marijuana users were less likely to have alcohol and other drug problems as compared to recreational marijuana users.
- Structural barriers in access to medical marijuana in the USA-a systematic review protocol
This 2017 protocol discusses disparities in medical marijuana access.
- Cannabinoids and Medical Marijuana: Clinical Considerations
This presentation from The Ohio State University Wexner Medical Center provides an evidence review of medical marijuana as a therapy. It also lists qualifying medical conditions for marijuana use in Ohio, adverse effects of marijuana use, and considerations that should be made if a patient requests medical marijuana.
- The Effects of Cannabis Among Adults With Chronic Pain and an Overview of General Harms: A Systematic Review
This 2017 study reviewed 27 chronic pain trials, 11 systematic reviews and 32 primary studies. The review found that very few studies were methodologically rigorous and these studies could not provide data on the long term health effects of medical marijuana use. The review also indicated that there was limited evidence on the adverse effects of marijuana use of the use of marijuana to decrease neuropathic pain. There was insufficient evidence on the use of marijuana to alleviate chronic pain.
- Medical marijuana research for chronic pain
This comment published in The Lancet in July 2017 calls for additional research on the health effects of medical marijuana use for those with chronic pain. It also cites legislation that hinder the progress of medical marijuana research.
- Nonmedical versus medical marijuana use among three age groups of adults: Associations with mental and physical health status
This 2017 study found that medical marijuana use was higher among the 50-64 age group than the young adult group. It also determined that more medical users than non-medical users had past-year marijuana use disorder and that, regardless of age, the odds of medical marijuana use were higher among those with marijuana use disorder and personality disorder.
- U.S. Epidemiology of Cannabis Use and Associated Problems
This accepted article preview from 2017 reviews existing research and statistics on the adverse health effects of marijuana use, trends in public perception, and the trends in potency and use. It evaluates the state of current marijuana laws and the relationship between these laws and marijuana trends. The article also provides a review of studies that evaluate marijuana use as a substitute for psychiatric medication and opioids or alcohol.
- Marijuana and Cannabinoids: A Neuroscience Research Summit
This meeting summary from a 2015 National Institutes of Health meeting provides an overview of the current research in marijuana use and neuroscience.
- Cannabis and Psychosis: a Critical Overview of the Relationship
A 2016 study showed that cannabis use does not cause psychotic disorders, but heavy marijuana use may be more common for those who are vulnerable to these disorders.
- Cannabinoids for Medical Use: A Systematic Review and Meta-analysis
This study, published in JAMA in June 2015, reviewed 79 trials on the benefits and adverse events of medical cannabinoid use. The review found moderate evidence of cannabinoids’ effectiveness in treating chronic pain and spasticity (muscle stiffness or rigidity). Other conditions analyzed, such as sleep disorders, nausea due to chemotherapy and Tourette syndrome, had low-quality or little evidence of effectiveness.
- Adverse Health Effects of Marijuana Use
This 2014 article from the New England Journal of Medicine reviewed available research on adverse health effects of recreational marijuana use by youth and adults, including addiction risk, effects on brain development, cancer risk, and impact on school and lifetime achievement.
- Systematic review and meta-analysis of cannabis treatment for chronic pain
This 2009 review found that marijuana is moderately effective as a treatment of chronic pain, but pain benefits are partially or completely offset by potential harms, such as changes in motor function, cognitive function, and perception (e.g. hallucinations).
- Adverse health effects of non-medical cannabis use
A 2009 study published in The Lancet examined 10 years of studies on regular marijuana use by adults and youth, looking at the findings on adverse effects
- Marijuana and Medicine: Assessing the Science Base
Issued by the Institute of Medicine in 1999, this book-length report summarizes potential medical uses and harms, effects on health and behavior, and varying delivery systems, among other subjects.
Impact on opioid addiction and overdose deaths
A 2014 study by Department of Veteran Affairs researchers found that laws legalizing medical marijuana use were associated with significant decreases in opioid overdose mortality. A 2015 working paper by the National Bureau of Economic also found that states permitting medical marijuana “experience a relative decrease in both opioid addictions and opioid overdose deaths compared to states that do not.”
- Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever
This 2017 article analyzes hospitalizations due to opioids and marijuana use with data from 1997-2014 state-level annual hospital discharge records. This study concluded that medical marijuana policies were significantly associated with a decrease in opioid pain reliever hospitalizations.
- Rationale for cannabis-based interventions in the opioid overdose crisis
This 2017 commentary in the Harm Reduction Journal uses the principles of the substitution effect to advocate for increased consideration for cannabis-based interventions in the opioid crisis. The author cites three windows of opportunity for these interventions: prior to opioid use for chronic pain, as a reduction method for those already using opioids for pain, and as an adjunct therapy to use during treatment for addiction.
Health effects of recreational/personal use
Although research has shown some association or correlation between recreational marijuana use and certain negative outcomes, it is important to note that researchers have not yet established direct causality. Additional longitudinal research is needed to determine whether adverse impacts are caused by marijuana use or related to other factors (social, mental, genetic, economic, etc.).
Youth initiation and use
Dependency
Studies have associated early marijuana use with increased risk of developing dependency and use of other illicit drugs. These risks increased with increased frequency of use and younger initiation.
- Likelihood of developing an alcohol and cannabis use disorder during youth: Association with recent use and age, 2008
- Cannabis Dependence: Its Nature, Consequences and Treatment, 2006
- Stages and pathways of drug involvement: Examining the gateway hypothesis, 2002
- Does cannabis use encourage other forms of illicit drug use?, 2000
- Reversible and regionally selective downregulation of brain cannabinoid CB1 receptors in chronic daily cannabis smokers, 2012
Cognitive, psychological and social development
Studies have found that youth marijuana use may impact certain areas of cognitive, psychological and social development. As with dependency, marijuana initiation and use at a younger age increased the strength of correlations with these developmental impacts.
- Speaking of Psychology: Marijuana: The brain changer, 2017
- Emotion regulation deficits in regular marijuana users, 2017
- Impulsivity, attention, memory, and decision-making among adolescent marijuana users, 2013
- Age of onset of marijuana use and executive function, 2012
- Effect of long-term cannabis use on axonal fibre connectivity, 2012
- Cannabis use before age 15 and subsequent executive functioning, 2011
- Gender effects on amygdala morphometry in adolescent marijuana users, 2011
- Altered prefrontal and insular cortical thickness in adolescent marijuana users, 2011
- Chronic cannabis users show altered neurophysiological functioning on Stroop task conflict resolution, 2010
- Functional MRI of inhibitory processing in abstinent adolescent marijuana users, 2007
Other impacts of marijuana use
- Prevalence and correlates of treatment utilization among adults with cannabis use disorder in the United States
This 2017 analysis of the 2005-2013 National Surveys on Drug Use and Health concluded that there was under-utilization of marijuana related treatment. The analysis also found that nicotine dependence and alcohol use disorder were both over 40% prevalent in young adults with cannabis use disorder. - No Detectable Association Between Frequency of Marijuana Use and Health or Healthcare Utilization Among Primary Care Patients Who Screen Positive for Drug Use
A 2013 study by Boston University found no association between frequency of marijuana use and healthcare utilization, comorbidities or self-reported health status in adults primary care patients who screen positive for drug use. - Prospective Study of Cannabis Use in Adolescents at Clinical High-Risk for Psychosis: Impact on Conversion to Psychosis and Functional Outcome, 2012
In this 2012 study, researchers found that low-to-moderate levels of lifetime marijuana use was not a major contributor to poor social or academic role functioning, according to existing data on at-risk youth. - Cannabis and educational achievement
A Journal of Addiction study published in 2003 found that marijuana use may decrease educational achievement. Researchers concluded that this outcome likely “reflects the effects of the social context within which cannabis is used rather than any direct effect of cannabis on cognitive ability or motivation.” - Marijuana-Using Drivers, Alcohol-Using Drivers, and Their Passengers: Prevalence and Risk Factors Among Underage College Students
This 2014 study found that, among marijuana-using college students, 44% of males and 9% of females drove after using marijuana, compared to 12% of males and 3% of female alcohol drinkers who reported driving after drinking. This study also includes numerous links to studies about crash risk of drivers under the influence, including youth drivers. - Pediatric Marijuana Exposures in a Medical Marijuana State
Colorado researchers found that accidental marijuana ingestion by children under 12 years old increased after marijuana possession laws changed in Colorado in 2009. An accompanying editorial in the JAMA Pediatrics volume cautioned that unintentional ingestion would likely increase as state marijuana possession and use laws become more permissive.
Marijuana use data
- Youth Risk Behavior Surveillance System (YRBSS)
This biennial survey conducted by the CDC includes national and state level data on marijuana among high school youth, including ever used, currently used, and tried before age 13. Trend data is available, and data can be sorted by race/ethnicity and grade level. - National Survey on Drug Use and Health (NSDUH)NSDUH is an annual survey of civilian, noninstitutionalized Americans aged 12 and older, conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA). The survey reports rates of drug, alcohol and tobacco use, including state and regional level data, and data broken out by age group. NSDUH data is also summarized in annual reports. The most recent report, 2015, is available here.
- Past 15-year trends in adolescent marijuana use: Differences by race/ethnicity and sexThis 2015 study published in the journal Drug and Alcohol Dependence provides an overview of trends in marijuana use among high school students, including demographic differences, through an analysis of data from the Youth Risk Behavior Survey (YRBS).
Health policy research and resources
- Controlled Substances Act, 21 U.S.C. § 812 (1996).https://www.fda.gov/RegulatoryInformation/LawsEnforcedbyFDA/ucm148726.htm#cntlsbb
- Ohio Revised Code (ORC) §3719.41
- ORC §3796.01 (B)
- The Rohrabacher-Farr Amendment. H.Amdt.748 to H.R.4660
- HB 523 amended Ohio Revised Code sections 109.572, 519.21, 4123.54, 4729.75, 4729.80, 4729.84, 4729.85, 4729.86, 4731.22, 4731.281, 4776.02, 4776.04, and 5713.30 and enacted Ohio Revised Code sections 3796.01, 3796.02, 3796.021, 3796.03, 3796.031, 3796.032, 3796.04, 3796.05, 3796.06, 3796.061, 3796.07, 3796.08, 3796.09, 3796.10, 3796.11, 3796.12, 3796.13, 3796.14, 3796.15, 3796.16, 3796.17, 3796.18, 3796.19, 3796.20, 3796.21, 3796.22, 3796.23, 3796.24, 3796.27, 3796.28, 3796.29, 3796.30, 4729.771, 4731.229, 4731.30, 4731.301, and 4731.302
- ORC §3796.02
- Section 3
- ORC §3796.03 (A)(1), §3796.04 (A)(1)
- ORC §3796.03 and 3796.04
- ORC §3796.01 (A)(6)
- ORC §3796.061 (A)
- OAC 4731-32-05(c)
- ORC §3796.06 (A)
- ORC §4731.30 (C)(2)
- ORC §3796.22 (B)
- OAC 3796:8-2-04(B)
- OAC 3796:7-3-01(A)
- “Marijuana Advisory panel Considers More Dispensaries.” The Hannah Report, April 20, 2017. http://www.hannah.com/DesktopDefaultPublic.aspx?type=hns&id=205412
- ORC §3796.22 (D)
- OAC 4731-32-02(C)
- ORC §4731.30 (C)(1)
- OAC 4731-32-02(A)(7)
- ORC 4731.30(H)
- ORC 4731.30(G)
- OAC 3796:6-5-01
- OAC 3796:6-2-05
- ORC §3796.05 (B)
- State of Ohio Board of Pharmacy. Dispensary Rules of Public Comment. Provided December 15, 2016. https://assets.documentcloud.org/documents/3239155/Dispensary-Rules-for-Public-Comment.pdf
- ORC §3796.04 (B)(9)
- Borchardt, Jackie. “185 apply for Ohio medical marijuana cultivator licenses.” Cleveland Plain Dealer, July 6, 2017. http://www.cleveland.com/open/index.ssf/2017/07/185_apply_for_ohio_medical_mar.html
- ORC §3796.28 (A)
- OAC 3796:6-3-10 (A)
- OAC 3796:6-3-11
